Lowering Cancer Risk Through Open Conversations
February 6, 2023
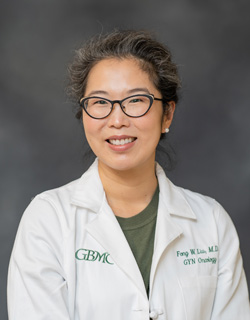
Fong Liu, MD, MPH, a gynecologic oncologist at the Sandra and Malcolm Berman Cancer Institute at GBMC and assistant professor at Johns Hopkins School of Medicine, wants more women to understand how their bodies work.
"I think it's very important for women to understand their anatomy and the nuances of cancer diagnosis and treatment," she explains.
She says this is especially true with uterine cancers like endometrial cancer, which makes up 90% of uterine cancer cases.
"The endometrium is the lining of the uterus. One of the greatest risk factors of endometrial cancer is obesity," says Dr. Liu. "As rates of obesity rise, we've also seen a rise in this type of cancer."
Obesity is a major risk factor for endometrial cancer because of how it affects two main hormones: estrogen and progesterone. Dr. Liu uses the analogy of growing grass to explain the role these hormones play in a cancer diagnosis.
"I like to think about estrogen as a fertilizer and progesterone as a lawn mower. There is a hormone in our fat cells that increases the level of estrogen in our bodies, which causes the lining of the uterus to grow faster than the progesterone can keep up. This uncontrolled overgrowth then leads to cancer development."
She adds that genetic factors are the other major risk factor for endometrial cancer, namely Lynch Syndrome, which is also associated with colon and ovarian cancer.
"Endometrial cancer is generally diagnosed in women in their 60s and 70s, but if you have risk factors and experience abnormal uterine bleeding at a younger age, please see your gynecologist for an exam," Dr. Liu says.
At this point, there are no general screening guidelines for endometrial cancer in the general population. "A biopsy done in the office can often make the diagnosis, and early diagnosis means we can hopefully remove it before it travels to other parts of the body."
"There will always be exceptions, but for most endometrial cancers, minimally invasive surgery is all you need to treat it," Dr. Liu says.
She adds that recovery depends on each person's cancer and what is found at the time of surgery, but many patients can go home the same day and recovery is straightforward.
"The most common post-surgery symptom is fatigue, and most patients have it for several weeks," Dr. Liu says.
Above all, Dr. Liu hopes normalizing conversations around gynecological cancers will encourage more women to take care of themselves before they get to the point of a cancer diagnosis.
"When you take care of a woman, you take care of her whole family because they're traditionally the caregivers. But also because of that, they often forget about themselves."
Dr. Liu's goal is to always support women by giving them a comfortable space to talk about their bodies. She encourages patients to get a second opinion if they feel like they aren't being heard.
By creating space for women to look at and talk about their bodies openly, Dr. Liu says they will feel empowered to take better care of themselves on every level.
"It hasn't been made okay to talk about these things. We need to make it okay."