Voice Disorders - Johns Hopkins Voice Center at GBMC
Voice Disorders
The cause of a voice disorder may be attributable to a wide range of structural, medical, neurological, or behavioral conditions. Complete evaluation by an otolaryngologist and a speech-language pathologist is highly recommended.
Acute Non-Specific Laryngitis
The term "laryngitis" refers to an inflammation of the vocal folds and larynx, and may cause hoarseness, lowered pitch, or even voice loss. Acute non-specific laryngitis may be associated with viral infections, acid reflux, exposure to pollutants in the atmosphere, exposure to tobacco or drugs, or a period of vocal fold irritation such as shouting.
Treatment:
Treatment is usually antibiotic or steroidal; occasionally voice therapy is recommended if appropriate.
Chronic Non-Specific Laryngitis
Chronic non-specific laryngitis refers to long-term inflammation of the vocal folds, and may be characterized by persistent hoarseness and vocal fatigue. Vocal overuse and misuse is a leading cause of chronic laryngitis. Additional causes include smoking, dehydration including the use of dehydrating medications, acid reflux disease, abusive use of mouth washes containing alcohol, or the repeated vomiting often associated with bulimia.
Treatment:
Varies depending on the cause. (The Voice and Its Disorders , Greene & Mathieson, 5th edition, Whurr Publishing, 1989). Voice Disorders Related to Vocal Overuse and Misuse

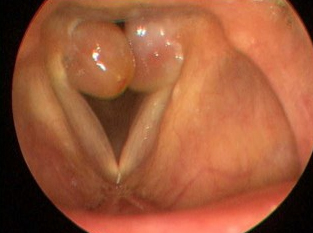
Vocal fold nodules are the most common benign vocal fold lesions, and are sometimes referred to as "singers nodes." They are usually bilateral and occur at the junction of the anterior 1/3 and posterior 2/3 of the vocal folds. They may vary significantly in size. Nodules may be acute or chronic; chronic, or "mature" nodules are similar to calluses within the vocal fold tissue. Vocal characteristics include hoarseness, breathiness, and lowered pitch.
Treatment: Voice therapy is often the first step in resolving nodules; treatment is usually 4 - 8 weeks. Results may vary depending on how long the nodules have been present and patient compliance with the therapy program. Surgical removal may be appropriate in some cases.

A vocal fold polyp is a fluid-filled lesion that may occur unilaterally or bilaterally. They may vary in size and will often be classified as either "sessile" (close to the tissue, like a blister) or pedunculated" (attached to a slim stalk). They are most commonly thought to be caused by vocal abuse or trauma, cigarette smoking, or vocal fold hemorrhage, but the exact cause is unknown. Vocal characteristics often include hoarseness, breathiness, diplophonia (audible perception of two distinct pitches), and stridor (noisy breathing).
Treatment: A vocal fold polyp usually does not respond to voice therapy; however, your physician may recommend voice therapy to clear the surgical field (reduce swelling and irritation). Surgical removal will most likely be recommended.
Vocal fold cysts are fluid-filled growths that may be congenital or acquired. They may appear on only one or both of the vocal folds. Vocal quality consistent with a vocal cord cyst may include hoarseness, breathiness, and voice and pitch breaks.
Treatment: Vocal fold cysts generally do not respond to voice therapy, and surgical removal will most likely be recommended depending on the severity of the vocal problem; however, your physician may recommend voice therapy pre-surgically to clear the surgical field (reduce swelling and irritation) or post-surgically to address any residual hoarseness.

Reinke's Edema occurs when the membranous portion of the vocal folds become filled with fluid. It may be unilateral or bilateral, and when it becomes very severe, it is often referred to as Polypoid Degeneration. Risk factors include long-term smoking and chronic vocal overuse or misuse. Vocal characteristics consistent with Reinke's Edema include significantly lowered pitch and severe hoarseness.
Treatment: Reinke's edema does not generally improve with voice therapy, and surgical removal is often recommended. Pre- or post-surgical voice therapy may be recommended by your physician.

Muscle Tension Dysphonia (MTD) is a general term to describe excessive and unnecessary tension of laryngeal muscles during voicing. MTD is often referred to by many different names, including hyperfunction, functional dysphonia, ventricular or false vocal fold compression, etc. MTD is often thought to be a compensatory mechanism in the presence of an underlying laryngeal pathology. Symptoms often include a sensation of excessive laryngeal tension and strain, vocal fatigue, and hoarseness.
Treatment: The definitive treatment for muscle tension dysphonia is voice therapy with a speech-language pathologist. Specific vocal exercises will be prescribed to decrease excessive muscular tension with voicing.

Vocal fold paresis (weakness) or paralysis (complete absence of movement) may result from a viral infection, cerebral vascular accident (stroke), trauma to the head, recurrent laryngeal nerve damage following surgery to the head, neck, or chest region, or may be idiopathic (cause unknown). A tumor may also cause immobility of the vocal fold(s). Vocal characteristics consistent with vocal fold paresis/ paralysis include breathiness, hoarseness, diplophonia (audible perception of two distinct pitches), decreased pitch range, and an inability to increase loudness.
Treatment: Treatment will vary depending on the cause of the paresis/ paralysis, but voice therapy and surgery are two common treatment options. Prior to any surgical recommendations, many physicians may request a procedure called a laryngeal electromyography to assess the nerve activity and recovery potential of the larynx.
Treatment: Spasmodic dysphonia has been known to be resistant to treatment. A popular treatment in the case of adductor spasmodic dysphonia are Botox injections. Botox, or botulinum toxin, is injected into certain laryngeal muscles to relax the muscles and decrease spasms. Voice therapy will not "cure" spasmodic dysphonia but is often recommended to educate the patient and to instruct the patient in compensatory strategies.

A hemorrhage of the vocal fold occurs when a blood vessel ruptures and bleeds into the submucosal layer of the vocal fold. A hemorrhage is usually unilateral, but can occur bilaterally, and is usually the result of a single episode of traumatic voice use. It may also result from a combination of overuse of the voice and taking anticoagulants (e.g., aspirin) or persistent usage of steroidal inhalants. Vocal characteristics include hoarseness, loss of pitch range, and vocal fatigue.
Treatment: Voice therapy is often recommended to address vocal health and hygiene and to instruct the patient in vocal facilitation techniques targeted at reducing swelling.
A varix is described as a long, defined blood vessel on the surface of the vocal fold, and is often seen in conjunction with a hemorrhagic episode. It is thought to be caused by vocal overuse or misuse and is usually the result of a single traumatic episode. Vocal quality may be hoarse.
Treatment: Voice therapy may be recommended depending on the vocal symptoms present.
Granulomas are vascular lesions that are most often the result of laryngopharyngeal reflux (acid reflux into the larynx), laryngeal intubation during surgery, or voice misuse. Because granulomas often occur on the vocal process of the arytenoid cartilage and not on the actual vocal fold, vocal quality may not be affected; however, vocal symptoms may include hoarseness, breathiness, reduced pitch range, and vocal fatigue.
Treatment: In cases where the granuloma is felt to be related to laryngopharyngeal reflux, anti-reflux medications are usually prescribed. Surgical removal may be necessary. Voice therapy is often recommended.

Papillomas are wart-like lesions thought to be caused by viruses. Lesions can invade deep into vocal fold tissue, causing severe hoarseness and breathiness, and in some cases, respiratory problems. Papillomas can occur throughout the larynx and upper airway.
Treatment: Because papillomas have a tendency to spread rapidly, surgical treatment is almost always recommended. Papillomas also have a tendency to recur, and often multiple surgical excisions are required. Voice therapy may be recommended to assist patients after surgery and to encourage optimal vocal quality.

A contact ulcer is a small lesion that typically develops on the medial portion of the vocal folds. The ulcer may be unilateral or bilateral. Contact ulcers are most often caused by vocal overuse and misuse, acid reflux into the larynx (laryngopharyngeal reflux), smoking, and excessive alcohol consumption. Vocal symptoms are often hoarseness, breathiness, lowered pitch, and decreased pitch range.
Treatment: As contact ulcers are often caused by laryngopharyngeal reflux, anti-reflux medication and diet and lifestyle modifications are typically recommended. Voice therapy is also often recommended to address vocal hygiene and behaviors.

Cancer may affect the oral, pharyngeal (throat), or laryngeal cavities. Most laryngeal cancers are of the squamous cell type, and are most often the result of chronic irritation due to cigarette smoke. Laryngeal cancer can be life-threatening, and can also cause devastating changes in voicing, breathing, and swallowing.
Treatment: Depending on the nature and severity of the cancer, treatment options include surgery, radiation, chemotherapy, or a combination of these therapies.

Normal aging of the larynx can result in loss of vocal fold tone and elasticity, resulting in hoarseness, breathiness, decreased loudness, and pitch instability. The hallmark appearance of presbylarynx is the appearance of "bowed" vocal folds secondary to vocal fold atrophy (muscle wasting).
Treatment: Voice therapy is often recommended to increase strength/ tone of laryngeal muscles, improve vocal fold closure, and improve overall vocal quality. In severe cases, an injection of a substance into the vocal folds may improve closure and quality.
